partner lymphocytes treatment
Almost 70 years ago, when the amazing mechanism of the human immune system was first described, Nobel Prize winning biologist Sir Peter Medawar made a significant remark.
He explained that the survival of the genetically different child in the womb was contrary to the immunological laws. Normally, the immune system recognises “foreign” tissue in the body and immediately builds up a defence against it (especially what is now called the “killer T-cell” mechanism).
Early experiments with organ transplants failed – the recipient’s immune system attacked the donor’s “foreign” organ tissue and rejected it.
But why does the womb not recognise the presence of the “foreign” tissue of the developing embryo and try to attack it?
Approximately 1 – 3% of all couples wanting children are affected by a habitual abortion. According to the WHO, this is defined as the occurrence of 3 or more successive miscarriages by the 20th week of pregnancy. The causes of this are many and varied, and in a large number of cases even remain unclear, so that immunological factors can be discussed, as the embryo represents a semi-allogenic transplant for the mother’s immune system, as half of the genes of the embryo are of paternal origin. Instead of a normal immune response, the embryo induces a secondary protective mechanism that contributes to successful implantation.
Immunisation with partner lymphocytes is a treatment option for recurrent implantation failure or recurrent miscarriage when all other possible causes have been excluded in advance. In immunisation with partner lymphocytes, the patient receives an intradermal injection of processed lymphocytes from her partner into the skin of the forearm to induce immune modulation or conditioning of the maternal (mother) immune system in accepting the paternal (father) antigens inherited from the embryo.

This form of treatment has been known for a relatively long time. Initially it was mainly used to treat patients with habitual abortions. Nowadays, many couples with unexplained sterility and unsuccessful efforts to achieve pregnancy are also being treated.
There is no standardised procedure for treatment. In our clinic the treatment is carried out with 2 sessions at intervals of 4 weeks. Approximately 3 weeks after the second immunisation, the so-called success control is carried out in the laboratory. The treatment is well tolerated; at the “vaccination site” a local allergic reaction, comparable to a severe insect bite, occurs. This subsides after about 10 days. General reactions are not to be expected. However, there are exclusions for the treatment method, so that it cannot be used for every couple.
Overall, the pregnancy rate can be increased by up to 20%. The probability of carry a pregnancy after treatment also increases by up to 30%, depending on the number of previous pregnancies. In our practice we have more than 25 years of experience with this treatment. Since the desire for a child has been successfully realised several times in a total of approx. 35% of the couples who have visited our consultation and treatment, the immunotherapy with partner lymphocytes still has a firm place in the treatment of infertility. The success is particularly evident in the first 6 months after the immunisation treatment, after which the chances of success decrease again. However, refresher treatments are possible.
Aktive Immunisierung mit Partnerlymphozyten bei Kinderwunschpatientinnen– der aktuelle Stand“ (Active immunisation with partner lymphocytes for fertility patients – the current status);
Veronika Günther, Ibrahim Alkatout, Wiebe Junkers, Nicolai Maass, Malte Ziemann, Siegfried Görg, Sören von Otte; Geburtsh Frauenheilk 2018; 78: 260–273 © Georg Thieme,Verlag KG Stuttgart · New York | ISSN 0016 5751
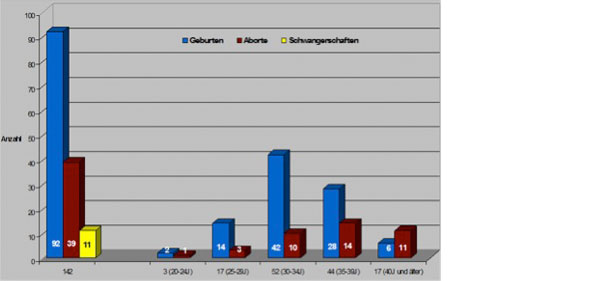
(Survey from 2005 – own patient clientele with habitual abortions)
(vocabulary: Geburten = births, Aborte = miscarriages, Schwangerschaften = Pregnancies)
